November 2019
RE: Routine Gynecologic Care
Dear Medicare Patient:
As you may already know, Medicare began paying for Annual Wellness Visits on January 1, 2011. In general, these visits should be performed by your primary care provider. The Medicare Annual Wellness Visit is designed to address your ongoing general medical needs and not routine/preventive gynecologic care or specific gynecologic problems. The services you normally receive at Advanced Women’s Healthcare (specifically, the pelvic and breast examinations and/or the collection of Pap smears) are not included in this Annual Wellness Visit.
Since 2011, AWH has accommodated our Medicare patients’ needs regarding routine/preventive gynecologic exams. This has resulted in a financial loss for the practice due to the fact that our services are considered “excluded” by Medicare. In other words, they are not a covered benefit on the plan. Due to this accommodation, we are considered “out of compliance” with Medicare regulations and will be making some necessary changes beginning January 2020.
Confused yet? We understand. Medicare can be confusing for all of us, even those of us in the healthcare field. Hopefully this letter and the excerpts of supporting documentation will clarify some of the logistics of Medicare and how it applies to you as our patient. Full access to these resources are located at the Medicare website (https://www.acog.org/-/media/Departments/Coding/Screening-Services-2018_final.pdf) and also on our website.
Effective January 2020, patients who choose to have their routine/preventive gynecologic exam with AWH will be required to pay an out of pocket fee at the time of service. This fee can range anywhere from $100-$250 to cover the (non-reimbursed) fees for the office visit. Your Medicare plan will be billed for the collection of pap smear (if applicable) and for your pelvic and breast exam. Your new Medicare Beneficiary Identifier (MBI) number and an updated, signed ABN form will be required at the time of check in. *Keep in mind, this out of pocket fee only applies for your routine/preventive gynecologic exam; ie: your “well woman exam”. This fee does not apply to visits addressing gynecologic problems/concerns.*
The following pages include:
- American College of OB-GYN (ACOG) Guidelines for Medicare Screening Services
- Medicare graphics/tools
- “Get Your New Medicare Card” flyer
If you have any questions, please feel free to call our Benefits Coordinator at 214-238-7808. We’re here to help.
Thank you,
The physicians and staff of Advanced Women’s Healthcare

Medicare Screening Services 2018
Although Medicare does not cover comprehensive preventive service visits such as those reported with CPT codes 99381-99397, Medicare continues to reimburse for certain screening services that are often performed during preventive service visits, including:
- Abdominal Aortic Aneurysm Screening
- Adult Immunizations
- Annual Wellness Visit (AWV), including Personalized Prevention Plan Services
- Bone Mass Measurements
- Cancer Screenings
- Cardiovascular Screening
- Diabetes Screening
- Diabetes Self-Management Training
- Diabetes Supplies
- Glaucoma Screening
- HIV Screening
- Initial Preventive Physical Exam (IPPE or “Welcome to Medicare” Physical Exam)
- Intensive Behavioral Therapy for Cardiovascular Disease
- Intensive Behavioral Therapy for Obesity
- Medical Nutrition Therapy (for Medicare beneficiaries with diabetes or renal disease)
- Screening and Behavioral Counseling Interventions in Primary Care to Reduce Alcohol Misuse
- Screening for Depression in Adults
- Screening for Sexually Transmitted Infections (STIs) and High Intensity Behavioral Counseling to Prevent STI
- Tobacco Use Cessation Counseling Services
NOTE: The frequency of coverage for screening services described below has not changed as a result of the advent of Medicare coverage for annual wellness visits.
Collection of Screening Pap smear Specimen
Medicare reimburses for collection of a screening Pap smear every two years in most cases.
The collection is reimbursed every year if the patient meets Medicare’s criteria for high risk. Following are the only criteria that are accepted by Medicare to indicate a high-risk patient:
- Woman is of childbearing age AND
- Cervical or vaginal cancer is present (or was present) OR
- Abnormalities were found within last 3 years OR
- Is considered high risk (as described below) for developing cervical or vaginal cancer
- Woman is not of childbearing age AND she has at least one of the following:
- High risk factors for cervical and vaginal cancer
- Onset of sexual activity under 16 years of age
- Five or more sexual partners in a lifetime
- History of sexually transmitted diseases (including human papilloma virus and/or HIV infection)
- Fewer than 3 negative or no Pap smears within the last 7 years
- DES (diethylstilbestrol)-exposed daughters of women who took DES during pregnancy
Screening Pelvic Exam
Medicare reimburses for a screening pelvic examination every two years in most cases.
This service is reported using HCPCS code G0101 (Cervical or vaginal cancer screening; pelvic and clinical breast examination). If the patient meets Medicare’s criteria for high risk, the examination is reimbursed every year. These criteria are the same as the ones listed above for the collection of screening Pap smear specimen. The diagnosis codes for Pap smear collection and screening pelvic exam are listed below.
A screening pelvic examination (HCPCS code G0101) should include documentation of at least seven of the following eleven elements:
- Inspection and palpation of breasts for masses or lumps, tenderness, symmetry, or nipple discharge
- Digital rectal examination including sphincter tone, presence of hemorrhoids, and rectal masses
- External genitalia (for example, general appearance, hair distribution, or lesions)
- Urethral meatus (for example, size, location, lesions, or prolapse)
- Urethra (for example, masses, tenderness, or scarring)
- Bladder (for example, fullness, masses, or tenderness)
- Vagina (for example, general appearance, estrogen effect, discharge, lesions, pelvic support, cystocele, or rectocele)
- Cervix (for example, general appearance, lesions or discharge)
- Uterus (for example, size, contour, position, mobility, tenderness, consistency, descent, or support)
- Adnexa/parametria (for example, masses, tenderness, organomegaly, or nodularity), AND/OR
- Anus and perineum
Screening for Cervical Cancer with Human Papillomavirus (HPV) Tests
HPV screening is recommended for all female Medicare beneficiaries who are asymptomatic and aged 30 to 65. Medicare reimburses for HPV screening once every 5 years.
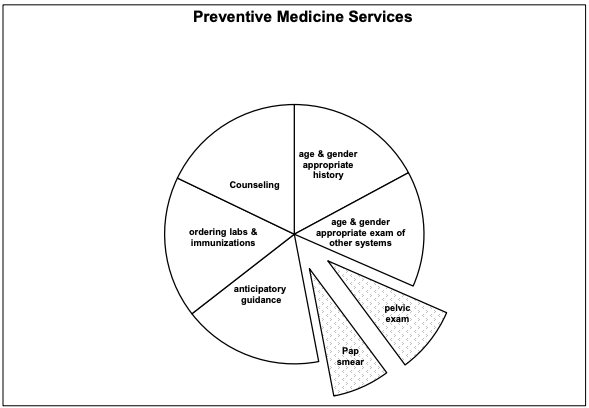
Medicare will reimburse for the shaded parts of the pie (the collection of the Pap smear and the pelvic exam). The remaining portions of the preventive service (office visit) are billed to the patient
GET YOUR NEW MEDICARE CARD
To help protect against identity theft, Medicare mailed new health insurance cards. Your new card has a new Medicare Number that’s unique to you, instead of your Social Security Number. To get your Medicare card:
- Call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048. There might be a problem that needs to be corrected, like updating your mailing address.
- Sign in to your MyMedicare.gov account. If you don’t have an account yet, visit MyMedicare.gov to create one. You can sign in to see your Medicare Number or print an official copy of your card.
Guard your Medicare card like it’s a credit card. Be sure to carry your card with you when you’re away from home. Let your doctor, hospital, or other health care provider see your card when you need hospital, medical, or other health care services